All Lives “Still” Matter. Understanding Different Experiences with the COVID-19 Depression among Foreign and Non-foreign Residents in Seoul, South Korea
Abstract
The pandemic has altered our lives, yet its impact is not equal for everyone. Some groups or individuals have experienced more severe effects, thus exacerbating health equity issues and contributing to long-term mental health problems. Specifically, foreign residents may be disproportionately affected by the COVID-19 pandemic compared to non-foreign residents due to the absence of a safety net and limited access to accurate COVID-19 information. While the importance of health equity at the city level has been highlighted, discussions on the differential experience of depression during the pandemic, particularly in Asia, remain sparse. This study explores the diverse factors influencing depression among foreign and non-foreign residents in Seoul, South Korea, based on a social survey of 7,500 residents (2,500 foreign and 5,000 non-foreign). Employing a partial least squares regression model, the findings indicate distinct patterns between the groups. Income-related indicators and the infodemic substantially affected depression in foreign residents, whereas social isolation, induced by the pandemic, impacted non-foreign residents. These disparate results underscore the necessity for tailored policy approaches to enhance health equity, particularly regarding economic support, social interaction, and access to precise information.
Keywords:
COVID-19 pandemic, Seoul, Depression, Foreign Residents, HealthⅠ. Introduction
The COVID-19 pandemic has prompted an economic downturn and triggered fears of disease infection in cities and regions (Chaudhary et al., 2021; Esterwood and Saeed, 2020; Kang et al., 2020; Ozili, 2020), which are associated with psychological distress and mental illness symptoms (Fancourt et al., 2021; Palgi et al., 2020). Mental health issues have continually increased as a result of the COVID-19 pandemic, while social interaction and opportunities for employment, education, and exercise, which could offset these risks, have decreased in our daily lives (Evans, 2020; Teychenne et al., 2017).
There has been growing recognition of the differential impacts of infectious diseases on various groups (or individuals), which affect health equity in the long term (Dimka and Mamelund, 2020; Farmer, 1996; Park, 2021). Those with little access to health services and a limited level of infection mitigation capacity may have a higher risk of experiencing serious symptoms (Farley et al., 2020; Shadmi et al., 2020). Some studies (Avato et al., 2010; Choudhari, 2020; Theng et al., 2020; World Bank, 2020) have indicated that foreign residents may be more severely affected by the COVID-19 than non-foreign residents, especially due to lack of safety nets and social protection in case of job loss or illness. Additionally, because of communication barriers, foreign residents are more likely to suffer from mental health problems such as depression (Gilmour et al., 2019; Heeren et al., 2014).
Although COVID-19 impacts depression in foreign and non-foreign residents differently, little research has explored factors that contribute to such a difference. Most research on mental health has focused mainly on vulnerable groups, such as those with underlying medical conditions (Lu et al., 2020), the elderly (Banerjee, 2020; García-Fernández et al., 2020), and medical staff (Spoorthy et al., 2020). Therefore, this research addresses the need for a comprehensive investigation of differential impacts on depression among foreign and non-foreign residents of cities during the COVID-19. Such an investigation is timely and appropriate given the increasing numbers of migrants and immigrants, particularly in Asia, where the pandemic originated. In practice, most previous research on health equity has focused on the West (e.g., Bartoš et al., 2021; Rye and Andrzejewska, 2010).
This study aims to examine varied factors that affect depression during the pandemic in foreign and non-foreign residents in Seoul, South Korea. Seoul was chosen as the city has seen a growing number of foreign residents, and it faced the issues of health equity between foreign and non-foreign residents (Hong and Lee, 2019; Lee et al., 2021a). We used a social survey of 7,500 residents (i.e., 2,500 foreign and 5,000 non-foreign residents) in Seoul. A partial least squares (PLS) regression model was used for empirical analysis, which was suitable for addressing multicollinearity and non-normality issues. Based on the survey findings, the research outlines policy recommendations that could enhance the mental health of both groups, thus contributing to health equity.
Ⅱ. Literature Review
1. Factors affecting mental health
TThe impact of COVID-19 on mental health is significant (Cullen et al., 2020; Pfefferbaum and North, 2020; Shinn and Viron, 2020). Prevention measures (e.g., lockdown policies), as well as the fear of COVID-19 infection and risk perception (Cullen et al., 2020; Xiong et al., 2020), have been found to significantly impact mental health (Killgore et al., 2020; Pietrabissa and Simpson, 2020). Public health studies suggest that people tend to show resilience after experiencing a disastrous event; however, some individuals with certain circumstances or specific characteristics (e.g., ethnic minorities and the elderly) may suffer from depression and anxiety (Chen, 2020; Pfefferbaum and North, 2020). Therefore, the impact of diseases and infection on mental health represents an important subject for research.
The factors affecting mental health during the pandemic include economic factors, voluntary and involuntary isolation, infodemic, and socio-demographic factors. First, economic factors such as income are closely related to the level of depression (Shinn and Viron, 2020). For example, lower economic status has been found to be associated with a higher prevalence of depression (Freeman et al., 2016). During the pandemic of COVID-19, the severe economic downturn that caused lower revenues and higher public expenditures, along with tightening financial conditions, has put pressure on the financial sustainability of governments, corporations, and individuals (UNDP, 2020). The economic impact has critical consequences for the ability to withstand and respond to shocks, especially of disadvantaged groups (Kang et al., 2020). Many authors (e.g., Carbone, 2020; Choudhury et al., 2021; Posel et al., 2021; Rohde et al., 2016) indicated that a decline in income, reduced employment and business opportunities, and employment insecurity result in a negative impact on people’s mental health.
Second, depression during the COVID-19 pandemic is related to involuntary isolation (e.g., social distancing ordered by lockdown policies) and voluntary isolation (e.g., social distancing practiced by individuals). Governments have implemented policies (e.g., social and physical distancing policies) to minimize individuals’ movement and contact with others, as the airborne transmission was considered the dominant route for spreading COVID-19 (Arroyo et al., 2021; Zhang et al., 2020). Many studies (e.g., Benke et al., 2020; Chaudhary et al., 2021; Sommerlad et al., 2021; Stickely and Koyanagi, 2016) identified that such policies for controlling COVID-19 have caused social and physical isolation, increasing levels of depression. Furthermore, voluntary isolation due to concerns regarding infection with COVID-19 (i.e., staying home voluntarily) also contributes to increasing depression (Mucci et al., 2020). Sommerlad et al. (2021) stated that people who used to be more sociable and empathetic have stronger depressive symptoms due to the lockdown and social distancing policies during the COVID-19 pandemic. Shin (2023) indicated that the more time spent alone during the pandemic, the greater the increase in feelings of depression, with men being more negatively affected than women, highlighting gender differences in impact. Yoon and Jin (2023) reported that the housing type affected individual depression levels differently during the COVID-19 pandemic, as the amount of time spent at home increased. For example, living in an apartment was shown to reduce depression during the pandemic period, with varying effects depending on gender and age.
Third, the infodemic can be on Shin (2023) found that the more time spent alone during the pandemic, the greater the increase in feelings of depression, with men being more negatively affected than women, highlighting gender differences in impact. Yoon and Jin (2023) reported that the characteristics of one’s home affected individual depression levels differently during the COVID-19 pandemic, as the amount of time spent at home increased. For example, living in an apartment was shown to reduce depression during the pandemic period, with varying effects depending on gender and age.e of the key factors affecting depression. According to World Health Organization (2021), infodemic means “too much information including false or misleading information in digital and physical environments during a disease outbreak”. As COVID-19 spread in many areas simultaneously, effective information delivery, digital enablement, and emotional contagion are considered important more than ever before (Larson, 2020; Naeem and Bhatti, 2020). In practice, mass media and social media have caused the infodemic relating to COVID-19, affecting the mental health of their users, rather than being useful platforms for promptly sharing accurate information (Gao et al., 2020; Toriumi et al., 2013). During the COVID-19 pandemic, depression is closely related to fake news and rumors mixed up in a large amount of available information on media, as well as excessive information that is accessible anytime on social media (Abdoli and Heidarnejadi, 2020; Xiong et al., 2020).
Fourth, the level of depression varies according to individuals’ socio-demographic characteristics, such as level of gender, education, age, and occupation (Xiong et al., 2020). Mamum and Ullah (2020) showed that poverty significantly affected depression and COVID-19 suicides, and there was a greater effect on fatality in women than men. Women have a higher risk for depression than men, which can be due to their higher sensitivity to the risk of disease infection (Gerhold, 2020; Gustafsod, 1998), greater employment instability, and higher housework time (Ge et al., 2020; Nwosu, 2021), and higher levels of pre-pandemic social interaction (Fagring et al., 2008; Han et al., 2021). Rudenstine et al. (2020) identified a negative correlation between depression and the household income of residents of cities. Depression decreased with higher levels of savings in the household. Furthermore, those with higher levels of education were found to be less affected by depression caused by COVID-19 (Nagasu and Yamanoto, 2020). Additionally, the younger generation had greater psychological distress than other age groups during the pandemic (Nagasu et al., 2021; Xiong et al., 2020).
2. Health equity in the context of COVID-19
A few studies have investigated health equity issues in mental health (e.g., psychological distress resulting from economic insecurity) (see Bas-Sarmiento et al., 2017; Qureshi et al., 2013). Pandemic-related psychological distress was noted among vulnerable populations in urban areas (Rudenstine et al., 2020). Several studies (Bourque et al., 2010; Lindert et al., 2008; Mindlis and Boffetta, 2017) reported that foreign residents have a higher risk of mental illness than non-foreign residents. Bas-Sarmiento et al. (2017) indicated that language, cultural, and administrative issues experienced by foreign residents may increase their vulnerability to physical and mental health problems. Ultimately, some foreign residents experience declining health status over time (Gushulak et al., 2011).
Achieving equitable access to health services across different groups is one of the crucial issues in health policy (Norredam et al., 2004). The exemplary policy responses during the COVID-19 include providing rescue packages, extending health insurance coverage, and increasing the production of personal protective equipment. The inequity in health services between foreign and non-foreign residents (e.g., differential level of emergency disaster relief supplies) seems greater than among non-foreign residents (Lee et al., 2021a). However, in practice, the current health policies in many countries fail to address such inequity issues (Machado and Goldenberg, 2021), while the number of immigrant workers increases across the globe (Green et al., 2007). For example, in South Korea, no medical care systems are made available for the systematic management and support of foreign residents’ health, although foreign residents who have lived in the country for more than six months are provided health insurance. (Lee et al., 2021a).
Overall, during a pandemic, non-foreign residents may experience varied issues related to language, cultural and administrative barriers, and inequity in health services, which together contribute to increasing the level of depression. However, comparative research of non-foreign and foreign residents, which explores conclusive evidence for differential impacts across these groups, is limited (Swinnen and Selten, 2007). Therefore, our research explores the factors influencing the mental health of these two groups and identifies policy implications for enhancing health equity during the pandemic.
Ⅲ. Research Design
1. Research area and data
Seoul, the capital city of South Korea was selected for this study. Out of 251,421 cumulative confirmed COVID-19 cases in the country, 79,354 occurred in Seoul, accounting for the largest proportion (31.6%) of all cities nationwide (KCDC, as of 2021). To respond to the spread of COVID-19, South Korea implemented personal preventive behaviors (e.g., wearing a face mask, keeping a 2-meter distance) and social distancing policies. These policies considered the vulnerability of urban spaces (e.g., multi-use facilities) to COVID-19, which typically spreads in 3Cs environments (closed spaces, crowded places, and close-contact settings) as noted by WHO in 2020. Based on the trends of COVID-19 spread, the policies progressively limited the use of multi-use facilities, the number of people gathering, and the hours of operation. By September 2020, when the survey was conducted, South Korea had experienced its first imported case of COVID-19 on January 20, 2020, followed by concentrated outbreaks in Daegu, Gyeongbuk, and the greater Seoul area from January 20 to August 11. Subsequently, a significant second wave of spread in the greater Seoul area occurred from August 12 to November 12, 2020, following a mass gathering in downtown Seoul and a cluster outbreak in religious groups on August 15, as reported by Yang et al. (2022).
The city has seen an increasing number of foreign residents, approximately 2,500,000, as of 2020 (KOSIS, 2021). About 22.7% of foreigners of various nationalities in South Korea reside in Seoul (Lee, 2020), being engaged in various types of occupations. As the city has an increasing number of foreign residents, health equity issues for foreign residents have been reported during the pandemic (Lee et al., 2021b).
The Seoul Metropolitan Government has been conducting the Seoul Survey annually since 2003, under the National Statistics authorization number 201011, to monitor the quality of life of its citizens. The 2020 Seoul Survey, utilized in this study, included items related to changes in the lives of residents due to the pandemic. Using the COVID-19 impact survey items, the study by Yoon and Jin (2023) analyzed the experiences of depression based on the type of residence during the pandemic. Data for the study was acquired and analyzed through the Seoul Open Data Plaza (seoul.data.go.kr).
A survey section for foreign residents was added in 2009. In the 2020 survey, COVID-19-related questions were newly introduced. Non-foreign residents in Seoul were sampled using stratified cluster sampling, while foreign residents living in Seoul for more than 91 days (excluding tourists) were sampled using stratified square root proportional sampling (by visa status and nationality, classified by duration of stay and gender). The sample used in the study was drawn to closely match the actual proportions of nationality, duration of stay, and gender reported by the foreign resident population in Seoul to the Ministry of Justice. The survey period was from September 14 to October 31, 2020, and was conducted through online surveys (non-foreign residents) and face-to-face interviews (both non-foreign and foreign residents) (The Seoul Metropolitan City, 2021). The 2020 data were used to compare the association between depression and various factors in two models, each of which comprised the subsamples of the foreign (n=2,500) and non-foreign (n=5,000) residents. Both models were designed to use identical items from the survey.
2. Input variables and methods
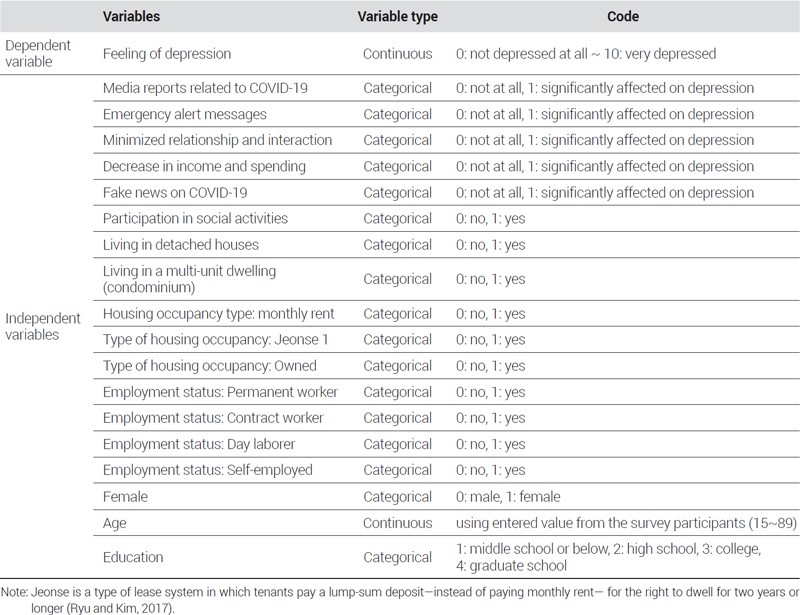
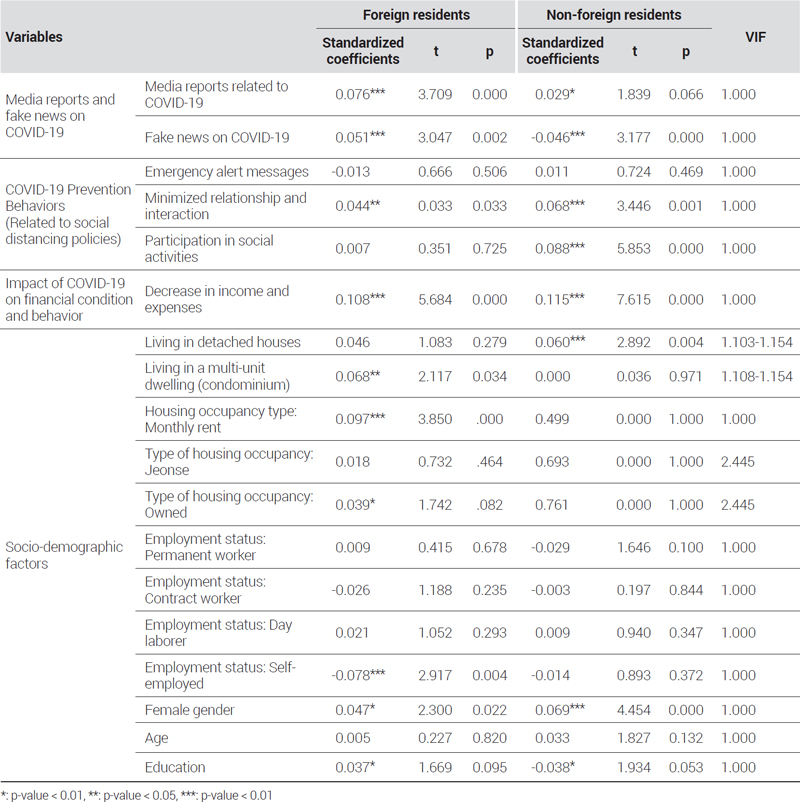
<Table 1> presents the variables that were identified as major stressors in the literature review. The dependent variable was a feeling of depression after the COVID-19 outbreak. To measure the variables, we used the following survey question: “Have you ever felt depressed in your daily life during the COVID-19 pandemic?” Responses were given on an 11-point Likert-type scale (0=not depressed at all to 10=very depressed). The independent variables included media reports related to COVID-19, emergency alert messages, minimized relationship and interaction due to social distancing, decrease in income and expenses, fake news on COVID-19, participation in social activities, gender (female), age, housing type (living in detached houses, and multi-unit dwellings), housing occupancy type (owned, jeonse, and monthly rent), employment type (permanent worker, contract worker, day laborer, self-employed), and education.1) In the category of ‘Employment type,’ those who are unemployed, students, housewives, and unpaid workers were marked as ‘0’ in the ‘Employment status’ section.
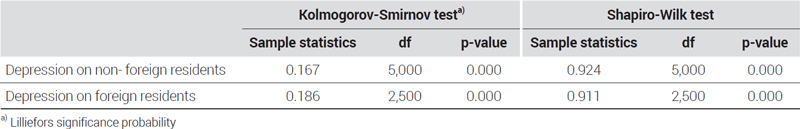
This study employed PLS regression instead of the traditional ordinary least squares (OLS) regression model in order to estimate the magnitude of the influence of the independent variables. PLS regression repeatedly outperformed both OLS regression analysis and exploratory factor analysis. The Kolmogorov-Smirnov and Shapiro-Wilk tests rejected the null hypothesis that the independent variable was normally distributed <Table 2>. Therefore, using OLS regression analysis was deemed unsuitable. As an alternative, PLS regression was adopted, as it functions well even when the data are severely non-normal. Furthermore, as noted earlier, PLS regression is useful for analyzing multiple variables, particularly when a model includes a large number of variables or with a high level of multicollinearity. PLS regression shares a common goal with OLS regression in modeling relationships and making predictions from data. However, the process of handling and predicting information differs between them. OLS is the most fundamental method used in regression analysis to identify a linear relationship between dependent and independent variables. On the other hand, PLS regression is akin to OLS regression. However, it proves to be a valuable analytical technique when dealing with multivariate data, particularly when there are more variables than observations and strong correlations among these variables.
Equation 1 shows the formula for PLS (Partial Least Squares) regression. PLS regression is a model that uses the linear combination of explanatory variables, where ‘t’ represents the linear combination in a situation with ‘n’ data points and ‘p’ explanatory variables.
| (1) |
PLS regression seeks the linear combination of independent variables that can best explain the dependent variable. It utilizes an axis that maximizes the quadratic form of the correlation vector between the variance of the linear combination of independent variables and the matrix of the dependent variable (Abdi, 2003).
Ⅳ. Results
1. Descriptive statistics
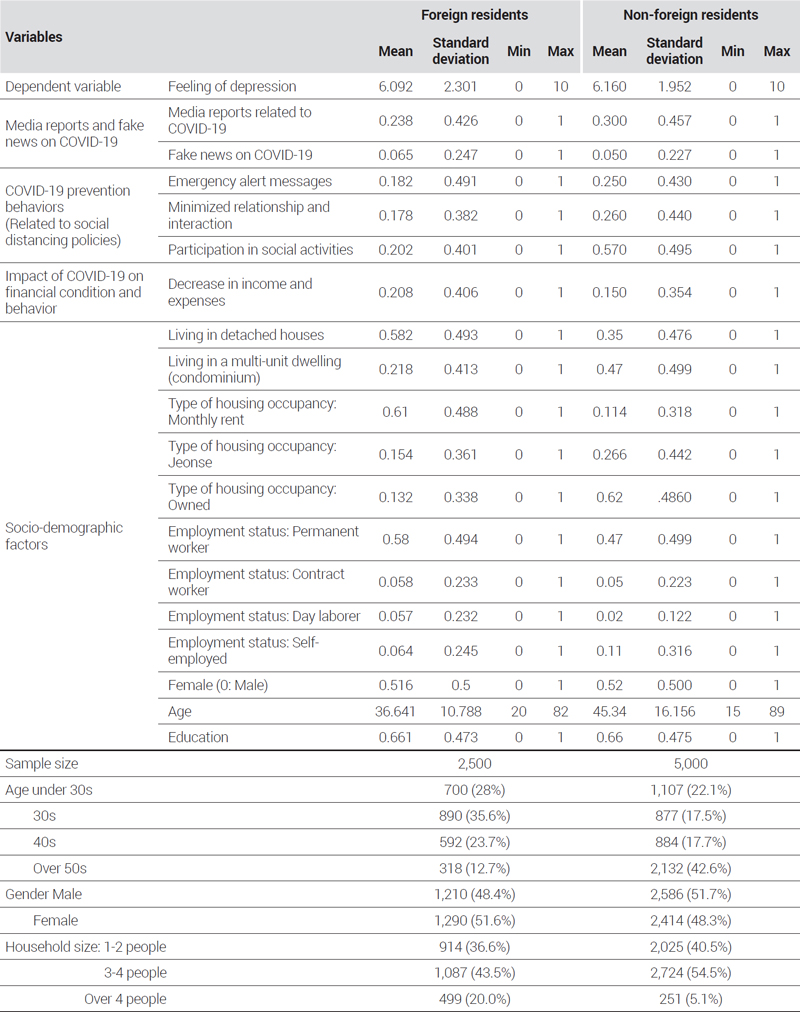
<Table 3> provides the descriptive statistics of the sample including the age, gender, and household size distributions of the foreign and non-foreign subsamples. During the pandemic, foreign and non-foreign resident groups felt similar levels of depression: 6.160 for non-foreign residents and 6.092 for foreign residents. The descriptive statistics of some independent variables showed substantial differences between the two sub-samples. Non-foreign residents evaluated participation in social activities (0.570) and minimized relationship and interaction (0.260) at a higher rate than foreign residents (0.202 and .178, respectively). Foreign residents evaluated a decrease in income and expense (0.208) and fake news on COVID-19 (0.065) higher than non-foreign residents (0.150 and 0.050, respectively). Among non-foreign residents, 20.3% (1,017 residents) live in detached houses, while 47.2% (2,358 residents) reside in apartments, the highest proportion. 32.5% (1,625 residents) live in multi-unit dwellings (townhouses and row houses). Meanwhile, among foreign residents, 14.8% (369 residents) live in detached houses, and 21.8% (545 residents) live in apartments. Additionally, 63.5% (1,586 residents) responded that they reside in multi-unit dwellings.
All variables showed sufficient variation for inferential statistics, for which this study consistently used the 95% confidence level.
2. Inferential statistics
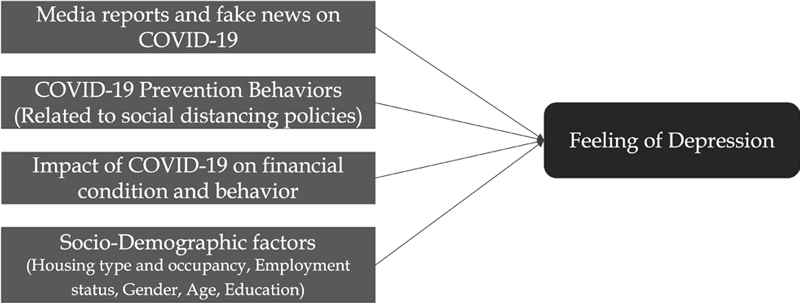
This study examined the 18 factors affecting depression during the pandemic through PLS regression. <Figure 1> demonstrates the structure of the research model. The variables named “Media reports and fake news on COVID-19”, “COVID-19 Prevention Behaviors”, “Impact of COVID-19 on financial condition and behavior”, “Socio-Demographic factors” corresponds to the independent variables represented for input purposes, which may affect feeling of depression, the dependent variable.
As shown in <Table 4>, the results indicated a substantial difference in factors affecting depression between the two groups. For foreign residents, decrease in income and expense (standardized path coefficient=0.108), monthly rent (0.097), being self-employed (-0.078), media reports related to COVID-19 (0.076), living in a multi-unit dwelling (0.068), fake news on COVID-19 (0.051), minimized relationship and interaction (0.044) were all found to be closely associated with depression during the pandemic.
Economic variables such as decreased income and expenses had the greatest impact on the level of depression for foreign residents. Among those who paid monthly rent, individuals with lower income might have experienced relatively a high level of depression. Self-employed people appeared to be less likely to be depressed. This could be because Seoul lowered the intensity of the social distancing policy at the time of the survey (September to October 2020) (Yeonhap, 2020). The respondents may not have experienced heavy losses from closing down their businesses. In this sense, differing results could be expected if the type of business—whether it is face-to-face or contact-free—was considered for the analysis. The model also showed that continual exposure to pandemicrelated information on media (e.g., fake news on COVID-19) affected the risk perception of foreign residents, increasing their depression level. This finding is in line with previous research on the relationship between mental health and social media exposure (e.g., Gao et al., 2020; Toriumi et al., 2013).
Among the socio-demographic factors, only gender (female) and living in a multi-unit dwelling (condominium) were significant for foreign residents. Females (0.047) experienced more depression than males during the pandemic, echoing the arguments of previous studies (e.g., Mamum and Ullah, 2020; Pieh et al., 2020; Xiong et al., 2020). Living in a multi-unit dwelling (0.068) was more likely to cause depression than other housing types.
For non-foreign residents, decrease in income and expenses (0.115), participation in social activities (0.088), minimized relationships and interactions (0.068), female gender (0.069), living in detached houses (0.060), fake news on COVID-19 (-0.046) were associated with the feeling of depression.
Decreases in income and expenses (0.115) were the most significant variables that affected the depression of non-foreign residents during the pandemic. The variables related to social interaction, such as participation in social activities (second strongest variables) and minimized relationship and interaction (third strongest variables), greatly impacted this group. The descriptive analysis showed that non-foreign residents are more likely to participate in social activities than foreign residents (see <Table 2>). Unlike foreign residents, fake news on COVID-19 (-0.046) appeared to reduce the level of depression among non-foreigners, the opposite of the results for foreign residents. It was also noted that the impacts of media reports related to COVID-19 on non-foreign residents were insignificant.
Female residents were more depressed than their male counterparts during the pandemic, as with foreign residents. These consistent results strengthen the findings of previous studies regarding the relationship between gender and COVID-19 depression (Gerhold, 2020; Vloo et al., 2021). Detached housing was associated with a higher level of depression for non-foreign residents, contrary to the fact that living in a multi-unit dwelling (condominium) brought about depression among foreign residents.
Ⅴ. Discussion and Conclusions
This study investigated differences in the factors affecting COVID-19-related depression between foreign and non-foreign residents using the case of Seoul, South Korea. Although both residents evaluated their degree of depression during the COVID-19 pandemic to be similar, this study found that the factors affecting depression varied in significance and magnitude.
The analysis of the result suggests that economic factors such as decreases in income and expenses as well as paying monthly rent can be strongly associated with depression during the pandemic, especially for foreign residents. Like many other disasters, the COVID-19 pandemic has resulted in substantial economic losses, leading to high unemployment and business closure rates (see Ozili, 2020; UNDP, 2020). The economic burden of purchasing protection measures tends to increase while access to health care services decreases particularly among vulnerable groups (Tai et al., 2020). With unequal access to health services and social protection in the context of an economic downturn, foreign residents can be at greater risk of having mental health problems (Karasapan, 2020). Thus, tailored alternatives are required to mitigate these varied detrimental impacts related to economic losses during the pandemic (e.g., temporary wage subsidy) (ISSA, 2020; OECD, 2020) to reduce the depression level of foreign residents.
Our research indicates that vulnerable living conditions during the pandemic may cause depression for foreign residents. In Seoul, multi-unit dwellings (e.g., condominiums), in which multiple people live together and share common spaces and facilities, appeared to increase the depression of foreign residents. Indeed, living in densely populated and closed spaces in cities increased the risk of COVID-infection (e.g., infection through air vents) even though there was no physical contact between residents (Han et al., 2021; World Health Organization, 2021; Zhang et al., 2020). To fundamentally tackle fear and depression induced by the pandemic, particular attention should be paid to comprehending the relation between types of housing and vulnerable living conditions for COVID-19 infection (Han et al., 2021; Kuang et al., 2020).
For non-foreign residents, variables related to social interaction such as social activity participation and social relationships can have a significant impact on their depression levels. As shown by the descriptive analysis (see <Table 2>), people who actively participated in social activities and had to minimize physical interactions due to the social distancing policies reported higher depression. Non-foreign residents may feel more affected by the restrictions on social networking than foreign residents because they are likely to have a wider social network and more social interaction. This finding contributes to the literature on mental health and social interaction (e.g., Pietrabissa and Simpson, 2020; Sommerlad et al, 2021) by clarifying the groups of individuals that the results of previous studies apply to, showing their relevance for non-foreign residents. The finding further highlights that while contact-free communication is expected to replace face-to-face interaction during the pandemic (Nguyen et al., 2021), social activities still assume an important role in facilitating effective communication. Specific policies to keep essential social activities during the pandemic should be considered in order to maintain the mental health of the urban population.
Living in detached houses can be also associated with high levels of depression, particularly for non-foreign residents, as they are likely to have a higher feeling of social isolation. Detached houses tend to have a smaller living space per household, in which one to two people reside (KOSIS, as of 2023). In this study, small households occupied 50.8% of detached houses, and most residents were in their 20’s and 30’s (see <Table 3>). When work, study, social interaction, and living all become integrated into the one place of home, due to involuntary and voluntary isolation (Kang et al., 2020), people living in detached houses could be more significantly affected by depression due to higher feeling of isolation. Single-person households face difficulties in dealing with illness, injury, adversity, social isolation, and loneliness (Shin, 2021), being more likely to have a higher level of depression (Benke et al., 2020).
Our study suggests that fake news related to COVID-19 has differential impacts on depression depending on individual characteristics and circumstances (Larson, 2020; Naeem and Bhatti, 2020; Toriumi et al., 2013), including the ability to comprehend information and accessibility to adequate information (Abdoli and Heidarejadi, 2020; Xiong et al., 2020). The substantial move to the information society has triggered the spread of fake news, such as false reports of confirmed cases through social media, affecting risk perception (Ahmad and Murad, 2020; Moscadeli et al., 2020; Larson, 2020). In the case of Seoul, such fake news increased the level of depression of foreign residents and decreased the depression of non-foreign residents. Compared with foreign residents, non-foreign residents are more likely to have a chance to check the credibility of fake news through various media channels or human networks. On the other hand, foreign residents may have difficulty verifying the information authenticity (Bailer et al., 2021) partially because of language barriers or limited social networks (Gilmour et al., 2019; Heeren et al., 2014; Wang et al., 2020). Consequently, fake news can raise concerns about the COVID-19 pandemic for foreign residents, leading to depression. In the vein, preventive measures are required to verify the authenticity of information and deliver accurate information, especially to foreign residents (e.g., see OECD, 2020; World Bank, 2020).
In short, the factors affecting depression in foreign and non-foreign residents of cities were varied in significance and magnitude. The impact of economic factors was graver for foreign residents while social isolation as induced by the pandemic appeared to affect non-foreign residents’ depression more profoundly. These varying results indicate that, under the same pandemic situation, factors affecting depression are different depending on resident characteristics. Minimized social interaction increases feelings of depression among both foreign residents and non-foreign residents, and the social isolation resulting from the COVID-19 pandemic exacerbates depression in non-foreign residents. In relation to this, the UK has implemented a social prescribing system that strengthens communities by connecting clients with link workers through remote counseling. This UK’s social prescribing service has been effective in reducing loneliness caused by over-reporting in the media due to COVID-19 and isolation due to public health policies, as shown by Younan et al. (2020).
Depression is affected by multiple factors and achieving equity in health among various groups requires measures to improve access to economic support, social interaction, and accurate information. Policy to enhance health equity can be developed based on understanding the different levels of adaptivity, vulnerability, and sensitivity of each group to varied socio-economic factors affected by the pandemic. For example, COVID-19-related policies should consider prioritizing economic supports, including emergency relief grants for foreign residents, as economic factors could affect the depression of these groups more severely. Moreover, as foreign residents may have different digital literacy compared to non-foreign residents, policy measures to deliver and manage accurate information must be considered. As noted in this study, foreign residents tend to refer to fake news without a chance to verify it, which can bring about depression. Jeong and Park (2021) revealed that many of the fake news reports filed from January to October 2020 were related to creating distortion and fear about the epidemic situation, COVID-19 policies, and international scenarios. In this context, while non-foreign residents experience a decrease in depression by identifying misinformation, foreign residents face limitations in discerning the authenticity of negative and distorted information, potentially increasing their depression. Subsequent research into the mental health problems that can arise from fake news, and the changes in depression based on the content (positive/negative) of the fake news, can be used in controlling the impact of fake news in future pandemic situations.
Amid growing international concern and policy recommendations for the mental health of foreign residents (e.g., Office for Health Improvement and Disparities, 2022/09/28; WHO, 2023/10/10), this study is significant for identifying that factors affecting depression during crises like pandemics differ between foreign residents and non-foreign residents. Particularly, this study enhanced its reliability by using survey data collected, considering the characteristics of the actual foreign resident population registered with the Ministry of Justice (gender, nationality, age, duration of stay), not for tourism purposes. This data can serve as a foundation for improving health equity in Asian regions with similar foreign resident characteristics. For future policy expansion, follow-up studies should compare and analyze the differences in factors affecting depression according to the duration of stay among foreign residents, considering the characteristics of migrants.
A limitation of this study is the potential for omitted variable bias, as general characteristics (e.g., personality) concerning depression were not considered due to the reliance on secondary data. Additionally, this study constructed models for both foreign and non-foreign resident groups to identify factors influencing depression during the pandemic in each group and compared these factors. Since the results were not compared using an integrated model, there are limitations in comparing the significant independent variables affecting each group on the same scale. Moreover, considering that past experiences with depression can influence its severity and impact during the pandemic, comparative studies with pre-pandemic periods are necessary. For a more detailed comparison, in-depth studies are required that conduct panel surveys at pre-pandemic, pandemic, and endemic stages to investigate the subjective perceptions of depression and its factors. As considerable time has passed since the beginning of the pandemic, further research is recommended to analyze the impact of vaccination and relaxed COVID-19 restriction standards. Furthermore, inasmuch, as this study was solely based on the case of Seoul, it is desirable to assess the replicability of its findings across different time, space, and population settings.
Acknowledgments
This work was supported by Seoul National University Research Grant in 2020 and under the framework of international cooperation program managed by the National Research Foundation of Korea(NRF-2020K2A9A1A01095494, FY2020).
References
- Abdi, H., 2003. “Partial Least Square Regression (PLS Regression)”, Encyclopedia for Research Methods for the Social Sciences, 792-795.
-
Abdoli, A. and Heidarnejadi, S.M., 2020. “Opportunities and Challenges of Social Media in Outbreaks: A Concern for Covid-19”, Ethics, Medicine and Public Health, 15: 100557.
[https://doi.org/10.1016/j.jemep.2020.100557]

-
Ahmad, A.R. and Murad, H.R., 2020. “The Impact of Social Media on Panic during the COVID-19 Pandemic in Iraqi Kurdistan: Online Questionnaire Study”, Journal of Medical Internet Research, 22(5): e19556.
[https://doi.org/10.2196/19556]

-
Arroyo, R., Mars, L., and Ruiz, T., 2021. “Activity Participation and Wellbeing during the Covid-19 Lockdown in Spain”, International Journal of Urban Sciences, 25(3): 386-415.
[https://doi.org/10.1080/12265934.2021.1925144]

-
Avato, J., Koettl, J., and Sabates-Wheeler, R., 2010. “Social Security Regimes, Global Estimates, and Good Practices: The Status of Social Protection for International Migrants”, World Development, 38(4): 455-466.
[https://doi.org/10.1016/j.worlddev.2009.10.003]

-
Bailer, W., Thallinger, G., Backfried, G., and Thomas-Aniola, D., 2021. “Challenges for Automatic Detection of Fake News Related to Migration”, Paper presented at 2021 IEEE Conference on Cognitive and Computational Aspects of Situation Management (CogSIMA), Tallinn, Estonia.
[https://doi.org/10.1109/CogSIMA51574.2021.9475929]

-
Banerjee, D., 2020. “‘Age and Ageism in Covid-19’: Elderly Mental Health-care Vulnerabilities and Needs”, Asian Journal of Psychiatry, 51(5): 102154.
[https://doi.org/10.1016/j.ajp.2020.102154]

-
Bartoš, V., Bauer, M., Cahlíková, J., and Chytilová, J., 2021. “Covid-19 Crisis and Hostility Against Foreigners”, European Economic Review, 137: 103818.
[https://doi.org/10.1016/j.euroecorev.2021.103818]

-
Bas-Sarmiento, P., Saucedo-Moreno, M.J., Fernández-Gutiérrez, M., and Poza-Méndez, M., 2017. “Mental Health in Immigrants versus Native Population: A Systematic Review of the Literature”, Archives of Psychiatric Nursing, 31(1): 111–121.
[https://doi.org/10.1016/j.apnu.2016.07.014]

-
Benke, C., Autenrieth, L.K., Asselmann, E., and Pané-Farré, C.A., 2020. “Lockdown, Quarantine Measures, and Social Distancing: Associations with Depression, Anxiety and Distress at the Beginning of the Covid-19 Pandemic among Adults from Germany”, Psychiatry Research, 293: 113462.
[https://doi.org/10.1016/j.psychres.2020.113462]

-
Bourque, F., van der Ven, E., and Malla, A., 2010. “A Meta-analysis of the Risk for Psychotic Disorders among First- and Second-generation Immigrants”, Psychological Medicine, 41(5): 897–910.
[https://doi.org/10.1017/S0033291710001406]

-
Carbone, S.R., 2020. “Flattening the Curve of Mental Ill-health: The Importance of Primary Prevention in Managing the Mental Health Impacts of Covid-19”, Mental Health & Prevention, 19: 200185.
[https://doi.org/10.1016/j.mhp.2020.200185]

-
Chaudhary, A.P., Sonar, N.S., TR, J., Banerjee, M., and Yadav, S., 2021. “Impact of the COVID-19 Pandemic on the Mental Health of College Students in India: Cross-sectional Web-based Study (preprint)”, JMIRx Med, 2(3): e28158.
[https://doi.org/10.2196/28158]

-
Chen, L., 2020. “Older Adults and COVID-19 Pandemic: Resilience Matters”, Arch Gerontol Geriatr, 89: 104124.
[https://doi.org/10.1016/j.archger.2020.104124]

-
Choudhari, R., 2020. “Covid 19 Pandemic: Mental Health Challenges of Internal Migrant Workers of India”, Asian Journal of Psychiatry, 54: 102254.
[https://doi.org/10.1016/j.ajp.2020.102254]

-
Cullen, W., Gulati, G., and Kelly, B.D., 2020. “Mental Health in the COVID-19 Pandemic”, QJM: An International Journal of Medicine, 113(5): 311–312.
[https://doi.org/10.1093/qjmed/hcaa110]

-
Dimka, J. and Mamelund, S., 2020. “1918 Influenza Outcomes among Institutionalized Norwegian Populations: Implications for Disability-inclusive Pandemic Preparedness”, Scandinavian Journal of Disability Research, 22(1): 175-186.
[https://doi.org/10.16993/sjdr.725]

-
Esterwood, E. and Saeed, S.A., 2020. “Past Epidemics, Natural Disasters, Covid19, and Mental Health: Learning from History as We Deal with the Present and Prepare for the Future”, Psychiatric Quarterly, 91(4): 1121-1133.
[https://doi.org/10.1007/s11126-020-09808-4]

-
Evans, M.K., 2020. “Covid’s Color Line — Infectious Disease, Inequity, and Racial Justice”, New England Journal of Medicine, 383(5): 408-410.
[https://doi.org/10.1056/NEJMp2019445]

-
Fagring, A.J., Kjellgren, K.I., Rosengren, A., Lissner, L., Manhem, K., and Welin, C., 2008. “Depression, Anxiety, Stress, Social Interaction and Health-related Quality of Life in Men and Women with Unexplained Chest Pain”, BMC Public Health, 8: 165.
[https://doi.org/10.1186/1471-2458-8-165]

-
Fancourt, D., Steptoe, A., and Bu, F., 2021. “Trajectories of Anxiety and Depressive Symptoms during Enforced Isolation due to Covid-19 in England: A Longitudinal Observational Study” The Lancet Psychiatry, 8(2): 141-149.
[https://doi.org/10.1016/S2215-0366(20)30482-X]

-
Farley, J.H., Hines, J., Lee, N.K., Brooks, S.E., Nair, N., Brown, C.L., Doll, K.M., Sullivan, E.J., and Chapman-Davis, E., 2020. “Promoting Health Equity in the Era of COVID-19”, Gynecologic Oncology, 158(1): 25-31.
[https://doi.org/10.1016/j.ygyno.2020.05.023]

-
Farmer, P., 1996. “Social Inequalities and Emerging Infectious Diseases”, Emerging Infectious Diseases, 2(4): 259-269.
[https://doi.org/10.3201/eid0204.960402]

-
Freeman, A., Tyrovolas, S., Koyanagi, A., Chatterji, S., Leonardi, M., Ayuso-Mateos, J.L., Tobiasz-Adamczyk, B., Koskinen, S., Rummel-Kluge, C., and Haro, J.M., 2016. “The Role of Socio-economic Status in Depression: Results from the Courage (Aging Survey in Europe)”, BMC Public Health, 16(1): 1098.
[https://doi.org/10.1186/s12889-016-3638-0]

-
Gao, J., Zheng, P., Jia, Y., Chen, H., Mao, Y., Chen, S., Wang, Y., Fu, H., and Dai, J., 2020. “Mental Health Problems and Social Media Exposure during COVID-19 Outbreak”, PLoS One, 15(4): e0231924.
[https://doi.org/10.1371/journal.pone.0231924]

-
García-Fernández, L., Romero-Ferreiro, V., López-Roldán, P.D., Padilla, S., and Rodriguez-Jimenez, R., 2020. “Mental Health in Elderly Spanish People in Times of Covid-19 Outbreak”, The American Journal of Geriatric Psychiatry, 28(10): 1040-1045.
[https://doi.org/10.1016/j.jagp.2020.06.027]

-
Ge, F., Wan, M., Zheng, A., and Zhang, J., 2020. “How to Deal with the Negative Psychological Impact of Covid-19 for People Who Pay Attention to Anxiety and Depression”, Precision Clinical Medicine, 3(3): 161-168.
[https://doi.org/10.1093/pcmedi/pbaa023]

-
Gerhold, L., 2020. “Covid-19: Risk Perception and Coping Strategies (preprint)”.
[https://doi.org/10.31234/osf.io/xmpk4]

-
Gilmour, S., Hoshino, H., and Dhungel, B., 2019. “Suicide Mortality in Foreign Residents of Japan”, International Journal of Environmental Research and Public Health, 16(17): 3013.
[https://doi.org/10.3390/ijerph16173013]

-
Green, C., Kler, P., and Leeves, G., 2007. “Immigrant Overeducation: Evidence from Recent Arrivals to Australia”, Economics of Education Review, 26(4): 420-432.
[https://doi.org/10.1016/j.econedurev.2006.02.005]

-
Gushulak, B.D., Pottie, K., Roberts, J.H., Torres, S., and DesMeules, M., 2011. “Migration and Health in Canada: Health in the Global Village”, Canadian Medical Association Journal, 183(12): E292-298.
[https://doi.org/10.1503/cmaj.090287]

-
Gustafsod, P.E., 1998. Gender “Differences in Risk Perception: Theoretical and Methodological Perspectives”, Risk Analysis, 18(6): 805-811.
[https://doi.org/10.1111/j.1539-6924.1998.tb01123.x]

-
Han, X., Chen, S., Bi, K., Yang, Z., and Sun, P., 2021. “Depression Following Covid-19 Lockdown in Severely, Moderately, and Mildly Impacted Areas in China”, Frontiers in Psychiatry, 12: 596872.
[https://doi.org/10.3389/fpsyt.2021.596872]

-
Heeren, M., Wittmann, L., Ehlert, U., Schnyder, U., Maier, T., and Müller, J., 2014. “Psychopathology and Resident Status – Comparing Asylum Seekers, Refugees, Illegal Migrants, Labor Migrants, and Residents”, Comprehensive Psychiatry, 55(4): 818-825.
[https://doi.org/10.1016/j.comppsych.2014.02.003]

-
Hong, J. and Lee, J., 2019. “Decomposing Income-related Inequalities in Self-reported Depression and Self-rated Health among Married Immigrants in South Korea”, International Journal of Environmental Research and Public Health, 16(10): 1869.
[https://doi.org/10.3390/ijerph16101869]

-
Jeong, D. and Park, J., 2021. “A Content Analysis of Covid-19 Fake-News: Pertaining to Disinformation and Its Manipulative Features”, Locality & Communication, 25(4): 216-258.
[https://doi.org/10.47020/JLC.2021.11.25.4.216]

-
Kang, M., Choi, Y., Kim, J., Lee, K. O., Lee, S., Park, I. K., Park, J., and Seo, I., 2020. “Covid-19 Impact on City and Region: What’s Next after Lockdown?” International Journal of Urban Sciences, 24(3): 297-315.
[https://doi.org/10.1080/12265934.2020.1803107]

-
Killgore, W.D. S., Cloonan, S.A., Taylor, E.C., and Dailey, N.S., 2020. “Loneliness: A Signature Mental Health Concern in the Era of COVID-19”, Psychiatry Research, 290: 113117.
[https://doi.org/10.1016/j.psychres.2020.113117]

-
Kuang, J., Ashraf, S., Das, U., and Bicchieri, C., 2020. “Awareness, Risk Perception, and Stress during the COVID-19 Pandemic in Communities of Tamil Nadu, India”, International Journal of Environmental Research and Public Health, 17(19): 7177.
[https://doi.org/10.3390/ijerph17197177]

-
Larson, H.J., 2020. “A Call to Arms: Helping Family, Friends and Communities Navigate the Covid-19 Infodemic”, Nature Reviews Immunology, 20(8), 449-450.
[https://doi.org/10.1038/s41577-020-0380-8]

- Lee, HY, 2020, Feb 17. “Over 2.5 Million Foreigners Residing in Korea for the First time in History...6.6%↑”, Yeonhap News.
-
Lee, J., Cho, S., and Jung, G., 2021a. “Policy Responses to covid-19 and Discrimination Against Foreign Nationals in South Korea”, Critical Asian Studies, 53(3): 432-447.
[https://doi.org/10.1080/14672715.2021.1897472]

- Lee, J., Kim, Y., and Lee, J., 2021b. “Discrimination Against Immigraints...Fifth Disaster Subsidy Does not Change”, Hankyeoreh, https://www.hani.co.kr/arti/society/society_general/1006510.html
-
Lee, S., Ong, A.R., Chen, C., and Elliott, M., 2020. “Respondent Driven Sampling for Immigrant Populations: A Health Survey of Foreign-born Korean Americans”, Journal of Immigrant and Minority Health, 23(4): 784-792.
[https://doi.org/10.1007/s10903-020-01077-4]

-
Lindert, J., Schouler-Ocak, M., Heinz, A., and Priebe, S., 2008. “Mental Health, Health Care Utilization of Migrants in Europe”, European Psychiatry, 23(S1): 14-20.
[https://doi.org/10.1016/S0924-9338(08)70057-9]

-
Lu, W., Wang, H., Lin, Y., and Li, L., 2020. “Psychological Status of Medical Workforce during the COVID-19 Pandemic: A Cross-sectional Study”, Psychiatry Research, 288: 112936.
[https://doi.org/10.1016/j.psychres.2020.112936]

-
Machado, S. and Goldenberg, S., 2021. “Sharpening Our Public Health Lens: Advancing IM/Migrant Health Equity during COVID-19 and Beyond”, International Journal for Equity in Health, 20(1): 57.
[https://doi.org/10.1186/s12939-021-01399-1]

-
Mamun, M. A. and Ullah, I., 2020. “Covid-19 Suicides in Pakistan, Dying off not Covid-19 Fear But Poverty? – The Forthcoming Economic Challenges for a Developing Country”, Brain, Behavior, and Immunity, 87: 163-166.
[https://doi.org/10.1016/j.bbi.2020.05.028]

-
Mindlis, I. and Boffetta, P., 2017. “Mood Disorders in First-and Second-generation Immigrants: Systematic Review and Meta-analysis”, British Journal of Psychiatry, 210(3): 182–189.
[https://doi.org/10.1192/bjp.bp.116.181107]

-
Moscadelli, A., Albora, G., Biamonte, M.A., Giorgetti, D., Innocenzio, M., Paoli, S., Lorini, C., Bonanni, P., and Bonaccorsi, G., 2020. “Fake News and Covid-19 in Italy: Results of a Quantitative Observational Study”, International Journal of Environmental Research and Public Health, 17(16): 5850.
[https://doi.org/10.3390/ijerph17165850]

- Mucci, F., Mucci, N., and Diolaiuti, F., 2020. “Lockdown and Isolation: Psychological Aspects of COVID-19 Pandemic in the General Population”, Clinical Neuropsychiatry, 17(2): 63-64.
-
Naeem, S.B., and Bhatti, R., 2020. “The Covid‐19 ‘Infodemic’: A New Front for Information Professionals”, Health Information and Libraries Journal, 37(3): 233–239.
[https://doi.org/10.1111/hir.12311]

-
Nagasu, M. and Yamamoto, I., 2020. “Impact of Socio-economic- and Lifestyle-related Risk Factors on Poor Mental Health Conditions: A Nationwide Longitudinal 5-wave Panel Study in Japan”, PLOS ONE, 15(10): e0240240.
[https://doi.org/10.1371/journal.pone.0240240]

-
Nagasu, M., Muto, K., and Yamamoto, I., 2021. “Impacts of Anxiety and Socio-economic Factors on Mental Health in the Early Phases of the COVID-19 Pandemic in the General Population in Japan: A Web-based Survey”, PLOS ONE, 16(3): e0247705.
[https://doi.org/10.1371/journal.pone.0247705]

-
Nguyen, M. H., Hargittai, E., and Marler, W., 2021. “Digital Inequality in Communication during a Time of Physical Distancing: The Case of COVID-19”, Computers in Human Behavior, 120: 106717.
[https://doi.org/10.1016/j.chb.2021.106717]

-
Norredam, M., Krasnik, A., Sorensen, T.M., Keiding, N., Michaelsen, J.J., and Nielsen, A.S., 2004. “Emergency Room Utilization in Copenhagen: A Comparison of Immigrant Groups and Danish-born Residents”, Scandinavian Journal of Public Health, 32(1): 53–59.
[https://doi.org/10.1080/14034940310001659]

-
Nwosu, C.O., 2021. “Childcare and Depression during the Coronavirus Pandemic in South Africa: A Gendered Analysis”, PLOS ONE, 16(8): e0255183.
[https://doi.org/10.1371/journal.pone.0255183]

-
Ozili, P.K., 2020. “Covid-19 Pandemic and Economic Crisis: The Nigerian Experience and Structural Causes”, Journal of Economic and Administrative Sciences, (ahead-of-print), 37(4): 401-418.
[https://doi.org/10.1108/JEAS-05-2020-0074]

-
Palgi, Y., Shrira, A., Ring, L., Bodner, E., Avidor, S., Bergman, Y., Cohen-Fridel, S., Keisari, S., and Hoffman, Y., 2020. “The Loneliness Pandemic: Loneliness and Other Concomitants of Depression, Anxiety and Their Comorbidity during the COVID-19 Outbreak”, Journal of Affective Disorders, 275: 109-111.
[https://doi.org/10.1016/j.jad.2020.06.036]

-
Park, J.H., 2021. “Who is Hardest Hit by a Pandemic? Racial Disparities in Covid-19 Hardship in the U.S.”, International Journal of Urban Sciences, 25(2): 149-177.
[https://doi.org/10.1080/12265934.2021.1877566]

-
Pfefferbaum, B. and North, C.S., 2020. “Mental Health and the COVID-19 Pandemic”, New England Journal of Medicine, 383(6): 510–512.
[https://doi.org/10.1056/NEJMp2008017]

-
Pieh, C., Budimir, S., and Probst, T., 2020. “The Effect of Age, Gender, Income, Work, and Physical Activity on Mental Health during Coronavirus Disease (COVID-19) Lockdown in Austria”, Journal of Psychosomatic Research, 136: 110186.
[https://doi.org/10.1016/j.jpsychores.2020.110186]

-
Pietrabissa, G. and Simpson, S.G., 2020. “Psychological Consequences of Social Isolation during COVID-19 Outbreak”, Frontiers in Psychology, 11: 2201.
[https://doi.org/10.3389/fpsyg.2020.02201]

-
Posel, D., Oyenubi, A., and Kollamparambil, U., 2021. “Job Loss and Mental Health during the COVID-19 Lockdown: Evidence from South Africa”, PLOS ONE, 16(3): e0249352.
[https://doi.org/10.1371/journal.pone.0249352]

-
Qureshi, A., Collazos, F., Sobradiel, N., Eiroa-Orosa, F.J., Febrel, M., Revollo-Escudero, H.W., Andrés, E., del Mar Ramos, M., Roca, M., Casas, M., Serrano-Blanco, A., Escobar, J.I., and García-Campayo, J., 2013. “Epidemiology of Psychiatric Morbidity among Migrants Compared to Native Born Population in Spain: A Controlled Study”, General Hospital Psychiatry, 35(1): 93-99.
[https://doi.org/10.1016/j.genhosppsych.2012.09.010]

-
Rohde, N., Tang, K.K., Osberg, L., and Rao, P., 2016. “The Effect of Economic Insecurity on Mental Health: Recent Evidence from Australian Panel Data”, Social Science & Medicine, 151: 250-258.
[https://doi.org/10.1016/j.socscimed.2015.12.014]

-
Rudenstine, S., McNeal, K., Schulder, T., Ettman, C.K., Hernandez, M., Gvozdieva, K., and Galea, S., 2020. “Depression and Anxiety during the COVID‐19 Pandemic in an Urban, Low‐income Public University Sample”, Journal of Traumatic Stress, 34(1): 12-22.
[https://doi.org/10.1002/jts.22600]

-
Rye, J.F., and Andrzejewska, J., 2010. “The Structural Disempowerment of Eastern European Migrant farm Workers in Norwegian Agriculture”, Journal of Rural Studies, 26(1): 41-51.
[https://doi.org/10.1016/j.jrurstud.2009.06.003]

-
Ryu, K.H. and Kim, J.A., 2017. “Jeonse, Will It Be Extinguished? Differentiation of Korean Rental Housing Market”, Journal of Housing and the Built Environment, 33(2): 409-427.
[https://doi.org/10.1007/s10901-017-9571-4]

-
Shadmi, E., Chen, Y., Dourado, I., Faran-Perach, I., Furler, J., Hangoma, P., Hanvoravongchai, P., Obando, C., Petrosyan, V., Rao, K.D., Ruano, A.L., Shi, L., de Souza, L.E., Spitzer-Shohat, S., Sturgiss, E., Suphanchaimat, R., Uribe, M.V., and Willems, S., 2020. “Health Equity and Covid-19: Global Perspectives”, International Journal for Equity in Health, 19(1): 104.
[https://doi.org/10.1186/s12939-020-01218-z]

-
Shin, A, 2023. “Changes in Time Use and Depression After COVID-19: Examining the Differential Effects in Men and Women”, Journal of Social Science, 34(1): 127-144.
[https://doi.org/10.16881/jss.2023.01.34.1.127]

- Shin, J., 2021, Apr 29. “Single-person Households in Seoul Outnumber Other Kinds”, The Korea Herald, http://www.koreaherald.com/view.php?ud=20210429000790
-
Shinn, A.K. and Viron, M., 2020. “Perspectives on the COVID-19 Pandemic and Individuals with Serious Mental Illness”, The Journal of Clinical Psychiatry, 81(3): 20com13412.
[https://doi.org/10.4088/JCP.20com13412]

-
Sommerlad, A., Marston, L., Huntley, J., Livingston, G., Lewis, G., Steptoe, A., and Fancourt, D., 2021. “Social Relationships and Depression during the COVID-19 Lockdown: Longitudinal Analysis of the COVID-19 Social Study”, Psychological Medicine, 52(15): 3381-3390.
[https://doi.org/10.1017/S0033291721000039]

-
Spoorthy, M.S., Pratapa, S.K., and Mahant, S., 2020. “Mental Health Problems Faced by Healthcare Workers due to the COVID-19 Pandemic–A Review”, Asian Journal of Psychiatry, 51: 102119.
[https://doi.org/10.1016/j.ajp.2020.102119]

-
Stickley, A. and Koyanagi, A., 2016. “Loneliness, Common Mental Disorders and Suicidal Behavior: Findings from a General Population Survey”, Journal of Affective Disorders, 197: 81-87.
[https://doi.org/10.1016/j.jad.2016.02.054]

-
Swinnen, S.G. and Selten, J.P., 2007. “Mood disorders and migration. British Journal of Psychiatry”, British Journal of Psychiatry, 190(1): 6-10.
[https://doi.org/10.1192/bjp.bp.105.020800]

-
Tai, D.B., Shah, A., Doubeni, C.A., Sia, I.G., and Wieland, M.L., 2021. “The Disproportionate Impact of Covid-19 on Racial and Ethnic Minorities in the United States”, Clinical Infectious Diseases, 72(4): 703-706.
[https://doi.org/10.1093/cid/ciaa815]

-
Teychenne, M., Abbott, G., Lamb, K.E., Rosenbaum, S., and Ball, K., 2017. “Is the Link between Movement and Mental Health a Two-way Street? Prospective Associations between Physical Activity, Sedentary Behaviour and Depressive Symptoms among Women Living in Socioeconomically Disadvantaged Neighbourhoods”, Preventive Medicine, 102: 72-78.
[https://doi.org/10.1016/j.ypmed.2017.07.005]

-
Toriumi, F., Sakaki, T., Shinoda, K., Kazama, K., Kurihara, S., and Noda, I., 2013. “Information Sharing on Twitter during the 2011 Catastrophic Earthquake”, Paper presented at WWW 2013 Companion - Proceedings of the 22nd International Conference on World Wide Web, Rio de Janeiro, Brazil.
[https://doi.org/10.1145/2487788.2488110]

- Theng, T.T, Nazhihah, M.N., and Jarud. R.K., 2020. Covid-19: We must Protect Foreign Workers, Khazanah Research Instittute.
- UNDP, 2020, June. “Socio-economic Impact”, Retrieved from https://www.undp.org/coronavirus/socio-economic-impact-covid-19
-
Vloo, A., Alessie, R.J. M., Mierau, J.O., Boezen, M.H., Mierau, J.O., Franke, L., Dekens, J., Deelen, P., Lanting, P., Vonk, J.M., Nolte, I., Ori, A.P.S., Claringbould, A., Boulogne, F., Dijkema, M.X.L., Wiersma, H.H., Warmerdam, R., and Jankipersadsing, S.A., 2021. “Gender differences in the mental health impact of the COVID-19 lockdown: Longitudinal evidence from the Netherlands”, SSM - Population Health, 15: 100878.
[https://doi.org/10.1016/j.ssmph.2021.100878]

-
Wang, C., Tian, Q., Zhao, P., Xiong, M., Latkin, C.A., Gan, Y., Hall, B.J., and Yang, B., 2020. “Disease Knowledge and Attitudes during the COVID-19 Epidemic among International Migrants in China: A National Cross-sectional Study”, International Journal of Biological Sciences, 16(15): 2895–2905.
[https://doi.org/10.7150/ijbs.47075]

- World Bank, 2020, Jun 19. “Potential Response to the COVID-19 Outbreak in Support of Migrant Workers”, https://documents1.worldbank.org/curated/en/428451587390154689/pdf/Potential-Responses-to-the-COVID-19-Outbreak-in-Support-of-Migrant-Workers-June-19-2020.pdf
- World Health Organization. “Infordemic”, Accessed Sep 30, 2021. https://www.who.int/health-topics/infodemic#tab=tab_1
-
Xiong, J., Lipsitz, O., Nasri, F., Lui, L.M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., and McIntyre, R.S., 2020. “Impact of Covid-19 Pandemic on Mental Health in the General Population: A Systematic Review”, Journal of Affective Disorders, 277: 55–64.
[https://doi.org/10.1016/j.jad.2020.08.001]

- Yoenhap, 2020, Oct 11. “S.Korea Eases Social Distancing to Lowest Level amid Coronavirus Downward Trend”, https://en.yna.co.kr/view/AEN20201011002353315
-
Yoon, C. and Jin. J., 2023. “Depression during the Covid-19 Pandemic: Are There Differences by Type of Housing and Housing Tenure?”, Housing Studies Review, 31(2): 73-108.
[https://doi.org/10.24957/hsr.2023.31.2.73]

-
Younan, H. C., Junghans, C., Harris, M., Majeed, A., and Gnani, S., 2020. “Maximising the Impact of Social Prescribing on Population Health in the Era of COVID-19”, Journal of the Royal Society of Medicine, 113(10): 377-382.
[https://doi.org/10.1177/0141076820947057]

-
Zhang, R., Li, Y., Zhang, A.L., Wang, Y., and Molina, M.J., 2020. “Identifying Airborne Transmission as the Dominant Route for the Spread of Covid-19”, Earth, Atmospheric, and Planetary Sciences. 117(26): 14857-14863.
[https://doi.org/10.1073/pnas.2009637117]

- ISSA, 2020, July 17. “COVID-19: Protecting Vulnerable Groups Through Emergency Benefits”, https://ww1.issa.int/analysis/covid-19-protecting-vulnerable-groups-through-emergency-benefits
- Karasapan, O., 2020, September 17. “Pandemic Highlights the Vulnerability of Migrant Workers in the Middle East”, BROOKINGS https://www.brookings.edu/blog/future-development/2020/09/17/pandemic-highlights-the-vulnerability-of-migrant-workers-in-the-middle-east/
- KCDC, 2021. “COVID-19 Outbreak Status”, http://ncov.mohw.go.kr/en/
- KOSIS, 2021. Foreign Residents by Municipality, https://kosis.kr/statHtml/statHtml.do?orgId=110&t-blId=TX_11025_A001_A&vw_cd=MT_ZTITLE&list_id=110_11025_2015_10&seqNo=&lang_mode=ko&lan-guage=kor&obj_var_id=&itm_id=&conn_path=MT_ZTITLE
- KOSIS, 2023, August 30. “Households (General Households) by Type of Housing Unit (including Office building) and Floor Area”, https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1JC1521&conn_path=I
- OECD, 2020, October 19. “What Is the Impact of the COVID-19 Pandemic on Immigrants and Their Children?”, https://www.oecd.org/coronavirus/policy-responses/what-is-the-impact-of-the-covid-19-pandemic-on-immigrants-and-their-children-e7cbb7de/